INTRODUCTION
Problem Description
The global prevalence of obesity is increasing at an overwhelming rate, and there are now more than 1.9 billion adults who are overweight or obese.1 Seventy-four percent of Americans are overweight and 41.9% are classified as obese.2 Body Mass Index (BMI) is a screening tool that is used to estimate the amount of body fat by comparing height to weight. A healthy BMI ranges from 18.5 to 24.9kg/m2. Elevated BMI is associated with an increase in cardiovascular disease, diabetes, and certain cancers, and overall mortality.3 Weight gain and a decrease in physical activity during nurse anesthesiology programs are known consequences of a stressful education.4 The exact amount of weight gain and decrease in physical activity among students was unknown. Therefore, the aim of this study was to investigate the impact nurse anesthesiology programs have on students’ weight and exercise levels and examine the methods students use to cope with increased stress.
Available Knowledge
A literature review was performed to examine the evidence on weight gain and physical activity during nurse anesthesiology programs. Pubmed, CINAHL, and Medline were searched. An initial search using keywords including stress, physical activity, weight gain, and nurse anesthesiology rendered zero results. A secondary search included keywords physical activity, weight gain, student, nursing student, and health care student yielded ninety-seven articles. This search was then filtered to include only studies focused on physical activity and weight gain among nursing or health care students, resulting in seven qualifying articles.
Results for students showed that decreased physical activity is linked to increased weight gain and BMI. Peterson, Sirard, Kulbok, DeBoer & Erickson3 found in a cross-sectional study of 94 university participants that sedentary behavior and lowered physical activity had a positive effect on BMI. They found that with each increase in number of sedentary extracurricular activities, the BMI increased by 0.930 kg/m2. Therefore, students who are not able to participate in physical activity are more likely to become overweight and/or obese.
A systematic review of almost 12,000 studies concluded that both undergraduate and graduate university students engage in an adequate level of physical activity and physical fitness.5 The university setting is an ideal environment to promote physical activity and wellness. However, other studies have showed that students enrolled in healthcare programs are at greater risk for having limited physical activity leading to an increase in BMI. A cross-sectional study by Blake, Stanulewicz, and McGill6 investigated the prevalence of physical activity among healthcare students. Of the 361 student respondents, 193 were enrolled in nursing programs and 168 were enrolled in medical school. They found that 48% of the nursing students and 39% of the medical students did not meet the recommended amount of physical activity. The reported barriers included that exercise was laborious, time-consuming, and caused fatigue. This is consistent with nurse anesthesiology programs which are known for their intensive and rigorous schedules.
Similarly, Lehmann, von Lindeman, Klewer, and Kugler7 found that one-quarter of the nursing students studied were overweight resulting from limited physical activity. They also concluded there was an increase in unhealthy behaviors like smoking and drinking during their time in nursing school. de Souza Urbanetto et al8 found that nursing students who exhibited stress stated they tended to eat more leading to weight gain.7
Lee and Kim’s9 study of 244 university students showed a link between increased sitting time and heightened levels of stress, anxiety, and depression. This is relevant for nurse anesthesiology students who face rigorous academic demands that require prolonged periods of sitting and studying. Mesisca and Mainwaring’s4 research further supports this, showing that as students’ well-being declines, their stress and anxiety levels tend to rise.
Specific aims
Evidence consistently shows that students who have limited physical activity are at an increased risk of becoming overweight and/or obese.3,6,7,10 Data shows that increased stress can also have a deleterious effect on weight gain and obesity.8 No studies looked specifically at the effects on students in nurse anesthesiology programs. The purpose of this study was to investigate the effect nurse anesthesiology programs had on the physical activity and weight gain of students who graduated from these programs and are now Certified Registered Nurse Anesthetists (CRNAs). The methods that students used to cope with increased stress was also examined to see if there was correlation between unhealthy coping mechanisms and weight gain.
METHODS
IRB Approval and Ethical Considerations
Prior to conducting this study, approval was obtained from the Institutional Review Board (IRB) at the University of North Florida. This ensured ethical standards were upheld to protect the respondents.
Intervention
An email requesting response in Survey Monkey, a third-party platform, was sent to current CRNA members of the Florida Association of Nurse Anesthetists (n=3595), excluding nurse anesthesiology students. The focus on practicing CRNAs rather than students ensured consistent tracking of weight gain throughout the program, avoiding issues with incomplete data. This approach also prevented additional demands on current students. The survey was distributed via email and responses were collected over eight weeks. No personally identifiable information such as names or email addresses was requested, ensuring anonymity. The use of the third-party platform facilitated this anonymous data collection. Participation was entirely voluntary, allowing respondents to engage without pressure or repercussions, which fostered an environment for honest feedback. Before beginning the survey, participants were informed about the study purpose, voluntary nature of their involvement, and how the data would be utilized.
Study of the Intervention
No validated survey tool was identified in the literature. Therefore, a unique survey was created. The survey included information for two key times in the participants’ education program: the beginning and at completion. The survey consisted of 33 questions: five questions were open-ended, two were dichotomous, five were checkbox, and twenty-one were Likert-scaled questions.
Measures
Data collected included age while in the program, gender, marital status, height, and weight. Other information collected investigated the consumption of alcohol, tobacco, and caffeine. Further information on stress level, frequency of exercise, and personal methods for coping with stress were collected. Information on participants’ nurse anesthesiology programs was also collected to determine the students’ beliefs on the level of care by the program for their mental wellness as well as if the program encouraged healthy activities.
Analysis
Descriptive statistics were used to organize the data, identify common themes, and determine where future research can be aimed. A Cronbach’s alpha test was conducted to assess the reliability of the Likert scale questions, which yielded a score of 0.7, indicating acceptable inter-reliability. Conversely, the Cronbach’s alpha for seven ‘how often’ Likert questions was lower at 0.5 which will be discussed in the limitation section.
RESULTS
A total of 352 CRNAs voluntarily completed the survey. Seventy-three percent of the respondents were female, 21% male and 6% chose not to disclose. The age of respondents ranged from 21-49. Of these respondents, 66% (n=232) reported experiencing weight gain during their education. The reported weight increase ranged from 0.52% to as much as 72%, with an average increase of 11%.
At the start of the nurse anesthesiology program, BMI values ranged from 18-46 kg/m2 per CRNA self-report. At completion of the nurse anesthesiology program, BMIs ranged from 17-48 kg/m2. Initially, 33% of participants (n=117) had a BMI of 25 kg/m2 or higher. This figure increased to 53% (n=185) by the end of the program. This shift indicates that over half of the respondents graduated with an unhealthy BMI, an increase of about one-third from the start of their education.
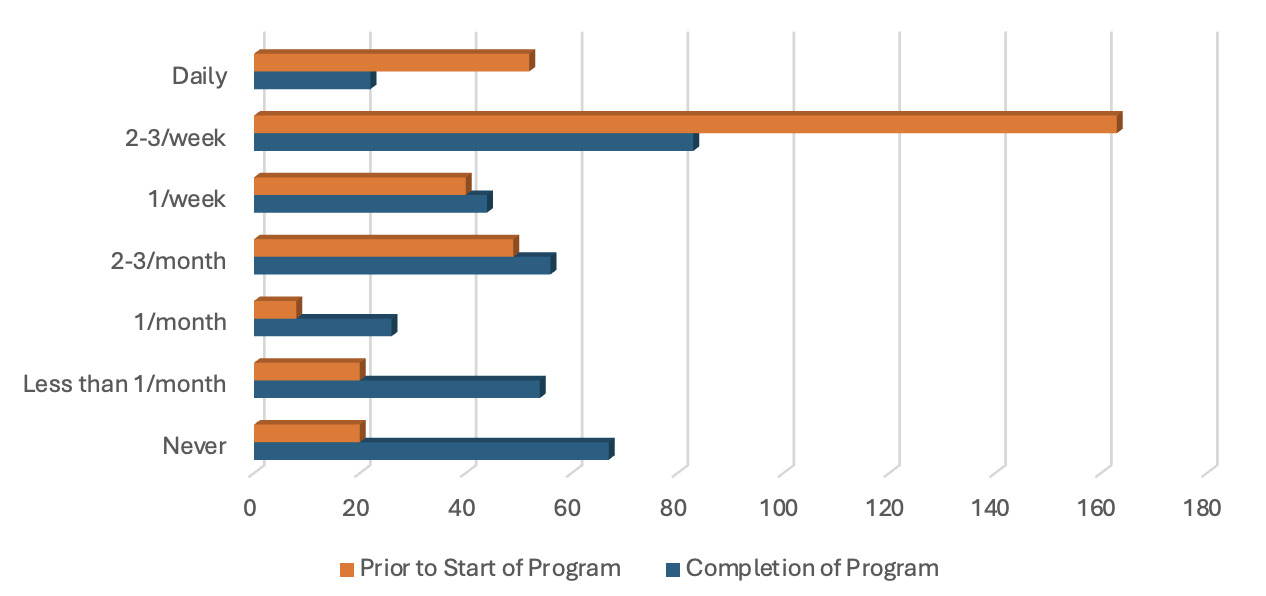
Consistent with findings from other studies, factors such as increased alcohol and tobacco consumption, poor eating habits, and reduced physical activity likely contributed to the observed weight gain. Prior to entering the nurse anesthesiology program, 65% of participants (n=219) reported exercising more than once per week. However, only 29% (n=102) managed to maintain this level of physical activity during the program (see Figure 1).
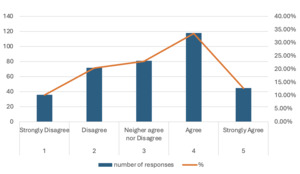
The majority (62%, n=218) of respondents reported decreased activity while in their nurse anesthesiology program. Also, 56% (n=196) reported using unhealthy eating as a coping mechanism while in the nurse anesthesiology program. Forty percent (n=139) reported increased alcohol consumption during their training program with 33% (n=115) reporting drinking alcohol two or more days per week. Sixteen percent (n=55) reported using tobacco at completion of their program, which was increased by 7% from those who used tobacco at the beginning. Seventy-seven percent (n=271) of respondents agreed that their nurse anesthesiology program was the most stressful undertaking they had ever experienced. Furthermore, 46% (n=162) agreed that it had a negative effect on their health (see Figure 2).
Only 34% (n=121) of the participants agreed that their school showed concern for their mental and physical well-being. The most common stressors of nurse anesthesiology programs identified by the survey results are the rigorous academic demands, high expectations of the student from themselves or others, anxiety regarding preparedness for the operating room, decreased time available for friends and family, and change in financial status. The most common stress-related symptoms included fatigue, somnolence, difficulty sleeping, and irritability.
STRENGTHS AND LIMITATIONS
Strengths of this study include the number of survey participants and the creation of topic-specific questions. Three hundred fifty-two CRNAs of the 3595 emailed responded to the survey which provided substantial data to analyze. This was a 9.7% response rate. The use of this survey tool allowed for data on specific information to be collected.
Limitations of this study include using self-reported information from participants. This can cause bias, especially if those who chose to respond were CRNAs who had significant effects on weight and health during their education. The data collected may not be reliable because participants answered retrospectively and most likely relied solely on memory. The Cronbach’s alpha test of the ‘how often’ Likert questions scored 0.5. Although this score was too low to establish reliability, it is important to note that the aim of this study was not to evaluate a comprehensive construct within nurse anesthesiology programs, but rather compare specific behaviors before and after the program completion. The survey tool was not formally validated, which raises concerns about the validity of the results. This should be considered when interpreting the findings as it shows the need for further research and refinement of the survey instrument in future studies.
DISCUSSION
The findings of this study highlight concerns regarding the health and well-being of nurse anesthesiology students. The reported prevalence of weight gain and reduced physical activity among respondents is concerning, particularly given the rigorous demands of the programs. As noted, 66% of participants experienced weight gain during their education, which transitioned into unhealthy BMI. This aligns with existing literature indicating stressful educational environments can detrimentally impact students’ health behaviors.
The correlation between increased stress levels and the adoption of unhealthy coping mechanisms necessitates addressing mental health in nurse anesthesiology programs. The fact that 77% of respondents identified their education as the most stressful experience of their lives suggests that the current educational structure needs to change to support students wholistically.
Implications for Nurse Anesthesiology Programs
Given these findings, it is crucial for nurse anesthesiology programs to implement strategies that prioritize student wellness, including the incorporation of structured wellness curricula that physical and mental health, stress management, and resilience training. By fostering a culture of health, faculty can help mitigate the negative health outcomes associated with the rigor of these programs. Additionally, creating supportive environments that encourage physical activity empowers students to make healthier choices, benefiting not only the students but also enhancing overall educational outcomes and cultivating healthier, more vigilant anesthesia providers. Future research should consider a longitudinal design with objective measures of physical activity and weight to strengthen the validity of the findings. Expanding the study to include programs throughout the United States would also provide a more comprehensive understanding of weight gain and physical activity in nurse anesthesiology programs.
Summary
The results of this study were consistent with other studies that time in rigorous and difficult programs limits physical activity and can contribute to weight gain. Most of the respondents had increased weight and decreased physical activity while in the program. Using unhealthy eating, alcohol, and tobacco as mechanisms to deal with stress can also contribute to the weight gain our participants disclosed. This study also showed that most respondents endured high levels of stress during their education with almost half of them stating there were deleterious effects to their health. With the known deleterious effects increased weight and obesity can have on health, action must be taken to minimize these in future nurse anesthesiology students. The survey also showed that most respondents did not believe that their program encouraged wellness or cared about their mental well-being. Therefore, it is suggested that nurse anesthesiology programs include wellness and health as a major focus of the program and outcomes. Program directors can include curriculum on health, exercise, and stress into their programs as well as encourage exercise and physical activity. By incorporating this into the program, hopefully, weight gain will be minimized, and physical activity will be maintained throughout nurse anesthesiology students’ education.