INTRODUCTION
Background and Literature Review
Peripheral intravenous catheters (PIVs) are the most commonly used invasive devices in hospitals, with approximately 300 million PIVs used every year in the United States.1 Approximately 80% of hospitalized patients and nearly all surgical patients require at least one PIV.2 In 1999, Keyes et al3 published the first study on the use of ultrasound to guide PIV insertions. Initially reserved as a last resort in difficult PIV cases, ultrasound-guided intravenous access (USGIV) is quickly becoming a standard of care.4 It is widely believed that an increase in ultrasound familiarity and availability will lead to routine ultrasound use in guiding PIV insertions, rather than being limited to a rescue tool.5
A systematic review and meta-analysis by Tran et al6 demonstrated that nurses using USGIV techniques for PIV placement achieved significantly higher first-attempt success rates compared to traditional landmark-based methods. A systematic review and meta-analysis by van Loon et al7 found that, compared to traditional palpation and direct visualization techniques, using an USGIV technique resulted in improved PIV insertion success rates, reduced the number of punctures, shortened the time to achieve IV access, and improved patient satisfaction. Additionally, because a reduction in failed PIV insertions saves staff time, decreases patient length of stay, and cuts costs, using an USGIV technique can be considered a cost-saving strategy.6,8,9
Bhargava et al10 found that after the implementation of a simulation-based USGIV course for pediatric intensive care nurses, catheters placed using an USGIV technique had higher first-attempt success rates and longer durations of use compared to catheters placed using traditional, landmark-based techniques. In a prospective cohort study of 238 nurses, Amick et al11 found that a simulation-based USGIV course improved nurses’ IV insertion skills and self-confidence. Finally, a systematic review by Hoskins et al9 found that competency in USGIV was not associated with an operator’s years of healthcare experience or professional role, whether nurse, physician, or allied health worker, but highlighted that simulation-based training is an effective method for developing USGIV skills.
Rationale, Purpose, and Aims
To keep nurse anesthesia programs at the forefront of anesthesia practice, the Council on Accreditation of Nurse Anesthesia Educational Programs mandated that, beginning January 1, 2022, all students entering an accredited nurse anesthesia program must complete a minimum number of successful vascular access attempts.12 Before this date, nurse anesthesia programs were not required to train students in the use of ultrasound guided access such as USGIV. Consequently, the first cohort of students graduating with mandatory ultrasound experience will enter the workforce in 2025. Many Certified Registered Nurse Anesthetists (CRNAs) currently in the workforce lack training in ultrasound-guided vascular access, including USGIV. Implementing a formal, standardized USGIV training course can bridge the knowledge and experience gap that these experienced CRNAs face.5,10,11
The purpose of this quality improvement (QI) project was to use a train-the-trainer model to educate a volunteer sample of CRNAs from a large anesthesia department in USGIV and evaluate the effect of the training on the knowledge, confidence, and skills of the CRNAs. The specific aims of the project were to adapt an existing USGIV course to the project’s setting, implement five sessions of the adapted course, and evaluate the effect of the training on the knowledge, confidence, and skills of the CRNAs. A secondary aim was to evaluate participant preference between a commercial and homemade USGIV trainer.
METHODS
Human Research Subjects Protection
Approval for this project was received from the University of Pittsburgh Human Research Protection Office (HRPO) (IRB # MOD20120005-004).
Setting
The setting for this project was the Post Anesthesia Care Unit (PACU) of a large, tertiary care academic hospital. A patient-free section of the PACU was reserved for the training. The target CRNA department for this QI project holds recurring 45-minute meetings every Wednesday morning before the first scheduled operating room cases. To avoid additional staffing hours, the training was conducted during these pre-scheduled meeting times.
Sample
A convenience sample of CRNA volunteers participated in this project. An IRB approved email script from the original USGIV course was emailed to CRNAs within the department, inviting them to voluntarily participate in the project and receive USGIV training. Certified Registered Nurse Anesthetists also had the option of receiving the same training without participating as subjects in the project.
Procedure
Adapted course
The original course, Ultrasound Advanced Practice Provider (USAPP) Peripheral IV Training, was developed at the Winter Institute for Simulation, Education, and Research (WISER) in Pittsburgh, PA.13 Originally 90-minutes in duration, this course was modified for this project to fit within the 45-minute timeframe of the scheduled Wednesday morning CRNA meetings. For a comparison between the original and adapted course, please refer to Table 1.
Train-the-Trainer Model
A train-the-trainer model was selected to support knowledge distribution and project sustainability. Ten second- and third-year volunteer Student Registered Nurse Anesthetists (SRNAs) were recruited as members of the research team and were trained by an experienced CRNA clinician in USGIV using the adapted USAPP Peripheral IV Training course. Immediately after completing their training, the 10 SRNA trainers conducted a practice session where they each trained additional SRNA volunteers who served as mock trainees. This allowed the 10 SRNA trainers to practice under the direct supervision of the supervising CRNA until deemed competent in deploying the curriculum.
This initial instructor preparation activity served two purposes: (1) preparing 10 SRNAs in a standardized and structured manner as course instructors to deploy a validated curriculum, and (2) as an initial “alpha test” of the adapted course. Lastly, a course debriefing was held, and minor modifications were made to improve the timing and efficiency of the adapted USGIV training course.
Commercial vs Tofu Phantom IV Blocks
Ultrasound-guided intravenous access insertions were performed using 20-gauge IVs on two types of vascular phantom IV blocks: commercial silicone block models (Your Design Medical, Brooklyn, NY) and homemade tofu models. The commercial models were purchased online for $249.99 per device, while the homemade tofu models cost was $2 per model.
To create the tofu phantoms, firm tofu blocks were purchased from a local grocery store. A chopstick was inserted into a thin balloon which was inserted horizontally through the tofu block, creating a “sandwich” effect. Four balloons were inserted into each tofu block to simulate vessels for cannulation. The balloons were filled with red-dyed water using a slip tip syringe and securely tied off.
CRNA Training Methods
Between January and March 2023, a series of five 45-minute courses were held, each accommodating 8-16 CRNAs. In these courses, one SRNA instructor trained two CRNAs, utilizing a single brand of ultrasound machine (Sonosite, FujiFilm Sonosite Inc., Seattle, WA). Upon arrival, each CRNA was provided with a tablet PC to take a pre-course survey and quiz and view a five-minute video outlining USGIV procedures.
The pre-course survey collected demographic information, including age, years of CRNA experience, and the frequency of IV insertions conducted monthly, both with and without ultrasound guidance. It also inquired about any prior ultrasound training and the participants’ confidence in their ability to perform USGIV procedures. The accompanying quiz assessed knowledge regarding the appropriate probe type for USGIV, necessary ultrasound adjustments (including depth and gain), and the ability to differentiate between arteries and veins. The demographics survey, knowledge assessment, and confidence assessment were all adapted from the original WISER course.
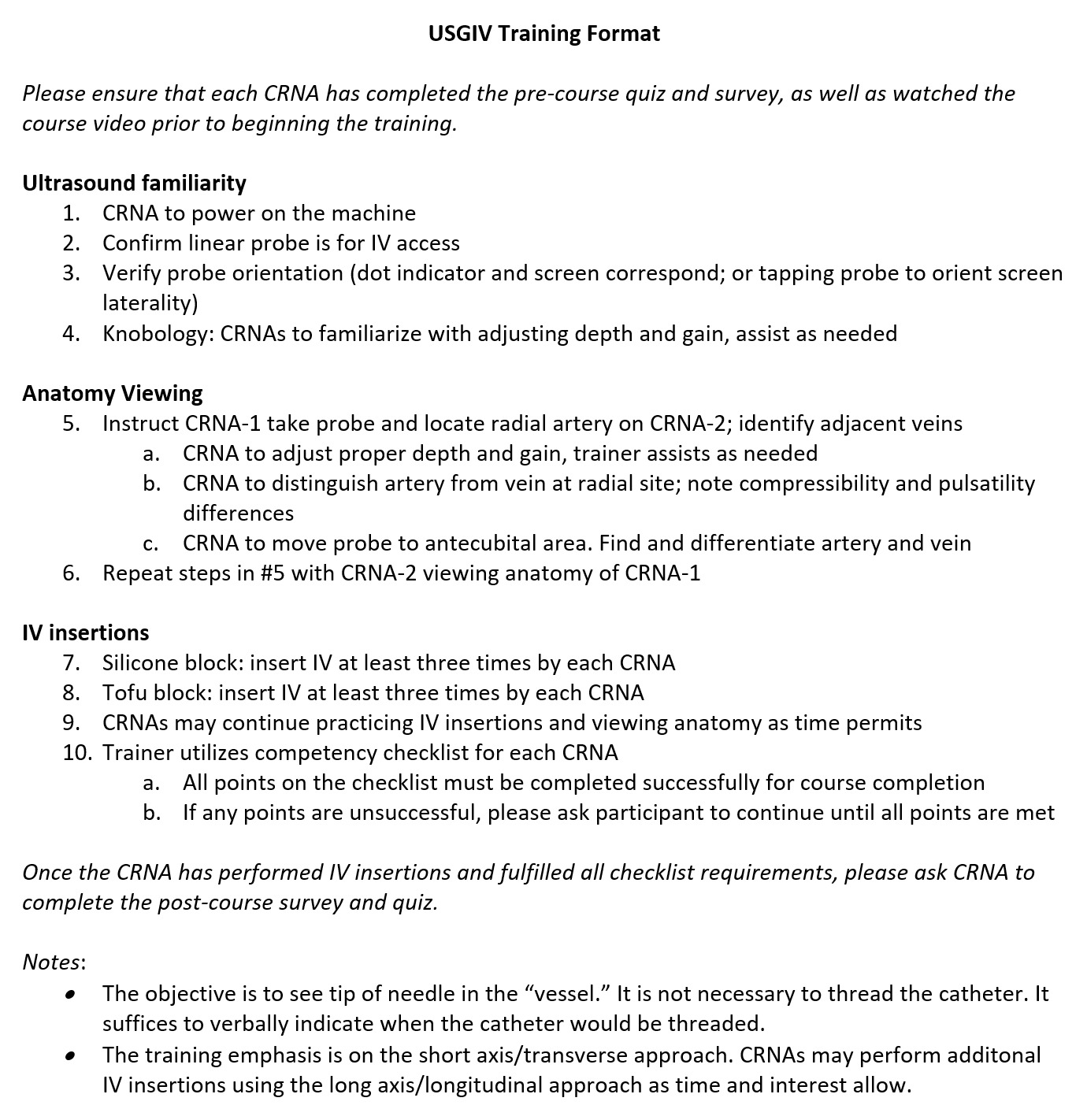
Following the completion of the pre-course assessments, CRNAs proceeded to their assigned ultrasound stations for hands-on training. Ultrasound-guided intravenous access cannulation attempts were made with 20-gauge peripheral IVs on both commercial and tofu vascular phantom blocks. A standardized training format was used to conduct the training as seen in Figure 2.
A skills competency checklist14 (Figure 3), previously validated by expert consultation, was used to verify CRNA skill proficiency.
Each checklist item was scored as completed or non-completed (according to specific operational guidelines), and redirection and retesting were provided until threshold competency was achieved on each checklist item (a course completion requirement).
While participants were required to achieve a minimum of six fully successful USGIV insertions for course completion, most performed several more. In total, CRNAs engaged in approximately 30 minutes of hands-on ultrasound training during each 45-minute course. The course culminated with a post-course quiz that was identical to the pre-course quiz. Additionally, a post-course survey was administered to gather feedback on various aspects of the course and evaluate whether participants preferred the commercial or tofu vascular phantom.
Data collection and Analysis
Both before and after the training sessions, every CRNA was provided with a tablet PC to complete pre-course and post-course surveys and quizzes. Delayed post-course surveys were sent via IRB approved emails to CRNA participants during the first, second, third, and fourth weeks following the course. All data were collected and stored securely within the WISER password-protected and encrypted Simulation Information Management System (SIMS) database.
De-identified data was distributed by an honest broker from the WISER database. Data analysis was performed using IBM SPSS Version 28.01.1. Descriptive statistics were used to describe demographic data, while assessments of knowledge and confidence levels were analyzed via Wilcoxon matched-pairs signed rank tests.
RESULTS
Demographics
From January to March 2023, 60 CRNAs participated in one of five courses throughout the project. The average age of participants was 39.5 (+/- 8.6) years, with an average of 10 years of CRNA experience. On a monthly basis, these CRNAs reported inserting an average of 43.6 IVs using standard palpation techniques, compared to just 1.1 IV insertions with ultrasound guidance. Notably, only 20% (12 CRNAs) had previously undertaken a formal ultrasound training course. Demographic information is detailed in Table 2.
Skills and Knowledge Assessment
All 60 CRNA participants met the course completion requirement of completing each item on the skills competency checklist for each of their six required insertion attempts. The average pre-course and post-course knowledge score improved from 5.0 to 7.3 out of 10, representing a 46% knowledge score improvement (Table 3). This change in mean knowledge score was statistically significant with a p-value < 0.01.
Confidence Assessment
The average pre-course and post-course confidence score improved from 36 to 74 using a 100-point confidence scale. This represented a 100.05% confidence score improvement (Table 4). The change in mean confidence score was statistically significant with a p-value = 0.002.
Commercial vs Tofu Phantom IV Blocks
A total of 32 CRNAs (53%) preferred using the silicone commercial phantom IV insertion ultrasound trainer, whereas 28 CRNAs (47%) preferred the tofu phantom. Although the commercial phantoms exhibited better resilience after multiple IV insertions, these models began to display artifact on ultrasound after 2-3 training sessions. This artifact occurred despite their advertised self-healing properties. The silicone models were, however, usable for all 5 courses. Conversely, the tofu phantoms withstood multiple IV sticks during one course but degraded significantly and were not usable for subsequent courses. Finally, the tofu phantoms required refrigeration, and a lengthier setup time compared to the commercial phantoms. For the comparison between the commercial and tofu phantoms, please refer to Table 5.
DISCUSSION
The purpose of this QI project was to implement a train-the-trainer model to educate a volunteer sample of CRNAs in USGIV and evaluate the effect of training on the knowledge, confidence, and skills of the CRNAs. A preexisting WISER course, USAPP Peripheral IV Training, was adapted for the project’s setting and timeframe. In total, 10 volunteer SRNAs were trained and participated as trainers, and 60 CRNAs participated in one of five courses conducted between January and March 2023. The average CRNA experience was 10 years with 80% (47 CRNAs) having had no prior formal ultrasound training.
Consistent with previous studies on simulation-based USGIV training,10,11 this project demonstrated positive effects on CRNA skills, knowledge, and confidence in USGIV. All 60 CRNAs successfully met the skills threshold requirement. The mean knowledge score showed a significant increase from pre-course to post-course, reflecting a 46% improvement. Additionally, the mean confidence score significantly increased, with a 100.05% improvement. However, only 24% (14) of CRNAs completed the post-course confidence assessment. The low response rate may be due to the confidence assessment’s exclusion from the immediate post-course survey and its inclusion only in the delayed surveys distributed weekly during weeks 1–4 post-course.
A secondary aim was to compare participant preference of the silicone commercial phantom block to the tofu phantom. All participants practiced with both models; 53% of CRNAs preferred the commercial phantom while 47% preferred the tofu phantom. The tofu phantoms remained functional for one course but degraded significantly and were not usable for additional courses. Conversely, the commercial phantoms were usable for all five courses but began to show signs of wear and artifact after 2-3 courses.
From a cost-effectiveness perspective, each commercial phantom cost 125 times the cost of a single tofu phantom, and it is unlikely that a commercial trainer would outlast 125 tofu phantoms. Despite the low cost of the tofu models, they required significant preparation time, needed refrigeration, and degraded quickly. This required 5-10 tofu models to be prepared for each course at a cost of $10-20 per session, not including preparation time. Therefore, although the tofu phantoms may be a more cost-effective option, further study is needed to more precisely define the cost-benefit relationship.
Limitations
One limitation of this QI project was the implementation of the confidence assessment, which was conducted weekly over four consecutive weeks post-course, but not included in the immediate post-course survey. This resulted in a response rate of only 24% (14 CRNAs). One potential improvement would have been to include the confidence assessment in the immediate post-course survey. Another limitation was the lack of assessment of the effect of the course on the SRNA instructors who participated in the project. This oversight presents an opportunity to assess the effect of the train-the-trainer model on the knowledge, confidence, skills, and change in ultrasound usage of SRNAs after participating in the project as a trainer. To address this, future courses can include a trainer assessment component. Lastly, this was a quality improvement initiative and thus the results cannot be generalized to other settings.
CONCLUSION
The use of USGIV is becoming increasingly recognized as a standard of care. The implementation of an USGIV training course can help bridge the knowledge and experience gap that many experienced CRNAs face in clinical practice. The development of this new skill positions CRNAs at the forefront of anesthesia practice and has the potential to improve patient satisfaction. This project demonstrated that a 45-minute USGIV course led to significant improvements in knowledge, confidence, and skills among experienced CRNAs who were trained by SRNAs utilizing a validated, structured, and standardized USGIV curriculum. The project received positive feedback from both CRNA practitioners and administrators.
Course materials were made available to participating CRNAs and SRNAs at the University of Pittsburgh through WISER. This project can serve as a model for CRNAs and future SRNAs to implement an USGIV course in other healthcare facilities. The use of tofu IV phantom blocks, which were favored by nearly half of the CRNAs, may represent a cost-effective strategy for conducting USGIV training, although the precise cost savings still need to be defined. Additional projects are needed to assess the effect of an USGIV course on CRNA knowledge, confidence, and skills at other facilities, as well as to assess changes in ultrasound use for this vascular procedure and for other procedures, such as central venous catheter and arterial line insertions.