Introduction
Ultrasonography is used by anesthesia providers for various procedures, from ultrasound-guided regional nerve blocks to point-of-care ultrasound. At our large midwestern academic hospital, ultrasonography has been underutilized by Certified Registered Nurse Anesthetists (CRNA) since most ultrasound procedures fall under the physician scope of practice at this institution. On January 30th, 2021, the Council on Accreditation of Nurse Anesthesia Educational Programs required ultrasound guided vascular access (USGVA) education be incorporated into nurse anesthesia program curriculum. The knowledge and skills nurse anesthesia students have developed in USGVA from their formal education prompted greater interest among the CRNAs of our institution to gain the education and experience needed to become proficient at this valuable skill. A prior survey at our institution revealed 52% of current CRNAs never received USGVA training during their formal anesthesia education and 64% never received USGVA training after their formal anesthesia education. The education and/or training CRNAs did report receiving was reported to be self-taught or peer guided. To succeed in ultrasound-guided procedures, proper education and experience are essential for CRNAs, particularly when encountering patients with difficult intravascular access.
This quality improvement (QI) project aimed to enhance ultrasound use for arterial and venous peripheral vascular procedures through the development and implementation of an online education module and hands-on simulation-based training. The primary aim was to increase the use of USGVA by 20% from baseline, with secondary aims of increasing knowledge, comfort, and confidence of CRNAs performing USGVA procedures.
Background
Obtaining reliable intravascular access is a fundamental skill for CRNAs. Venous cannulation is essential for administering medications, fluids, and blood products and arterial cannulation is often required for continuous arterial blood pressure monitoring and laboratory testing.1–4 Traditionally, CRNAs identify target vessels using landmark techniques, relying on presumed anatomical location, surface anatomy, and manual palpation.1,3–16 Difficult intravascular access is associated with extremes of chronological age, obesity, diabetes, intravenous drug use, end-stage renal disease, vascular pathology, hypovolemia, and hypotension among other factors.1–4,6–11,17 Difficult intravascular access often leads to multiple attempts, decreased patient comfort and satisfaction, increased need for central venous access, and treatment delays.1,2,5–8,11,16
Real-time ultrasound guidance enhances the likelihood of successful cannulation on the first attempt.2–4,16–22 Ultrasound guidance is also associated with shorter time to successful cannulation, greater patient satisfaction, and fewer complications.4,5,7,11,13,14,17,19,20,22 This demonstrates why ultrasound is now the standard of practice for central venous access, given the complications that may occur without it.5,6,10–12,14 By providing real-time, 2-dimensional imaging of anatomical structures, ultrasound offers a more objective assessment than traditional methods of palpation and direct visualization.14 Ultrasound enables the CRNA to assess suitable vascular targets through visualizing anatomical variations such as changes in vessel size, bifurcations, thromboses, calcifications, as well as vessel’s relation to neighboring structures such as nerves and other vasculature.12,14,21,23 Given the rise in obesity in the United States, the demand for ultrasound guidance in identifying deeper vessels has become necessary.7,11,12 Many institutions recommend that only qualified personnel with adequate ultrasound training use ultrasound guidance for peripheral vascular access procedures.4,6,11 For hands-on procedures like USGVA, providers are encouraged to complete sufficient training, including didactic instruction, simulation-based practice, supervised skill performance in the clinical setting, and performance evaluations.4,6,11,19
Previous studies on USGVA education have incorporated didactic education coupled with hands-on competency assessments to demonstrate proficiency.6,11,16,19–21 For instance, Bhargava et al6 studied a group of nurses performing first and second attempt peripheral intravenous (PIV) cannulation on pediatric patients using traditional landmark techniques. After completing a 1 hour didactic session and hands-on training in ultrasound-guided PIV access, the nurses achieved statistically significant improvements in PIV success rates with an increase from 47.3% to 85.9% for first attempts and 54% to 92.2% for second attempts.6
Competency thresholds varied among studies. For example, Adhikari et al9 deemed learners to be competent once they demonstrated successful cannulation on a simulation model, while Anderson et al8 measured competence after at least 9 successful cannulations post-education.6 Note that when introducing a new technique, practice and experience are necessary to achieve competence. Ultrasound-guided vascular procedures require fine motor skills and precise hand-eye coordination to guide the needle tip into a vessel which can be challenging for novice practitioners that are not familiar with ultrasound.11
Methodology
This QI project was deemed exempt from Institutional Review Board approval and supported by the anesthesia department’s clinical practice committee. The primary goal was to increase ultrasound use by CRNAs for peripheral vascular access procedures, with secondary goals of enhancing ultrasound knowledge, comfort, and confidence in USGVA.
Step One: Needs Assessment
A needs assessment survey was distributed via the internal Research Electronic Data Capture (REDCap) system to all CRNAs within a large, midwestern academic hospital and was completed by 50% of CRNA staff. CRNAs who reported difficult intravascular access (1-2 times/month: 52%; 3-5 times/month: 26%; 5 or more times/month: 18%) rarely chose to utilize ultrasound (never: 39%; 1-2 times: 38%; 3-5 times: 11%; 5 or more times: 11%). Eighty-five percent of the CRNAs who completed the survey agreed or strongly agreed that proficiency in USGVA is a necessary skill of CRNAs, however 58% felt they did not have the training or experience necessary to perform USGVA independently. Ninety percent of the CRNAs indicated interest in formal ultrasound education and hands-on training for USGVA.
Step Two: Online Module Development
The use of ultrasound for any procedure requires knowledge of ultrasound technology, sonoanatomy, ultrasound transducer orientation, and proper body ergonomics. An online module was created with the help of institution-supported medical photographers, medical animation specialists, and instructional designers specializing in education. The module was divided into 4 lessons and took approximately 60 minutes to complete.
The first lesson covered ultrasound technology and physics. An interactive video provided an overview of ultrasound frequency, soundwave reflection, and attenuation artifact affecting soundwave transmission. The 3 most common ultrasound transducers, linear, curvilinear, and phased array, were discussed including ultrasound frequency, ultrasound wave distribution, and common uses for each transducer. The high frequency linear transducer was designated as the preferred ultrasound transducer for USGVA, since it provides the best resolution of small structures less than 6 centimeters in depth.
The second lesson focused on vascular anatomy, including the most common venous and arterial anatomical structures within the upper extremity. Examples of the expected sonoanatomy and anatomical relationships of veins, arteries, and nerves, and the echogenic differences between these structures were also provided. Anatomical knowledge of arteries and veins is crucial for the CRNA to identify the specific target vessels in a systematic and timely manner. It is equally important for the CRNA to know the location of surrounding structures to prevent iatrogenic complications during vascular access procedures.
The third lesson covered ultrasound machine preparation. The lesson provided interactive images on machine set up allowing the participant to practice adding patient information, choosing the appropriate linear transducer, and positioning the ultrasound machine to allow proper ergonomics for the provider. The last portion of this lesson included a video on proper sterile sheath application of the transducer.
The final lesson included instructions on how to orient the transducer to the ultrasound screen and how to scan the target vessel and surrounding anatomy. Once the vessel was identified, the learner was instructed to optimize image resolution by adjusting gain and depth and demonstrate proper transducer mechanics to center the vessel on the ultrasound screen. Lastly, while holding the ultrasound transducer with the nondominant hand and catheter/needle with the dominant hand, 2 styles of dynamic out-of-plane techniques were demonstrated via videos.
For shallow vessels (< 0.5 cm deep), the tilting technique was demonstrated starting with the transducer tilted toward the insertion site to visualize the needle tip prior to vessel puncture. Once the needle tip is identified as a hyperechoic dot on the ultrasound screen, the transducer is tilted away from the insertion site to follow the needle tip into the vessel. For deeper vessels (> 0.5 cm deep), the sliding technique was demonstrated starting with the transducer perpendicular to the skin. Once the needle tip is identified, the transducer is slid away from the insertion site, stopping when the needle tip is no longer identified on the ultrasound screen. The needle is then advanced until it reappears, and this sliding process is repeated until the needle tip is guided into the vessel. The final portion of this lesson demonstrated how to save an image for proper electronic medical record documentation.
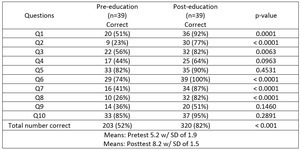
Included in the education module was a pre- and post-education test to measure knowledge acquisition. The questions for the pre- and post-test were the same. To measure the change in participant knowledge, the pre-test answers were not released. Once the learner completed the online module and post-test, the questions and answers were shared with the learner for review.
Step Three: Hands-on Simulation-based Training Development
Three simulation stations were created to measure the learner’s understanding of the educational material and allow an opportunity for hands-on practice. The first station included anatomical identification of specific structures of the upper extremity via ultrasound. Each CRNA was asked to identify various veins, arteries, and nerves on a human volunteer including: the cephalic vein of the forearm, the basilic vein of the upper arm, the radial artery at the wrist, the ulnar nerve at the wrist, the brachial artery at the cubital fossa, and the median nerve at the cubital fossa. The other 2 stations measured the learner’s ultrasound technique when cannulating arterial and venous structures on gel models using the dynamic short-axis, out-of-plane technique. Participants had the choice of using either the tilting or sliding technique for each station. The hands-on training allowed participants to practice these techniques on artificial models under instructor guidance before utilizing these techniques in clinical practice. Participants used institution-provided ultrasound machines and a linear transducer for each station.
Step Four: Implementation
To support statistical significance, a sample size of 30 volunteers was deemed sufficient as a participant group. Given the possibility of some CRNAs not completing portions of the project, the goal for the initial group of CRNA participants was 50 volunteers. Seventy-nine CRNAs replied to an email invitation volunteering to participate in the project. Fifty CRNAs were randomly selected using a random draw generator, representing all 10 specialty practice areas. Of the 50 volunteers invited to participate, 39 completed every aspect of the project including pre- and post-surveys, the educational module, and in-person simulation training.
Prior to assigning the online education, a survey was sent to the study group via REDCap to assess their current estimated use of USGVA over the span of 1 month, confidence in their knowledge of ultrasound, comfort with using the technology, and any barriers encountered to the use USGVA. Once the survey was complete, they were assigned the online module and were asked to complete the module including the pre- and post-tests within 2 weeks. The hands-on simulation-based training was held on 2 separate days and CRNAs used their personal time to participate. This training was conducted within a large conference room setting where 3 stations were set up for each skill. Each volunteer spent 30 minutes completing the 3 stations and received 1:1 observation and instruction. Three months after participants completed the education, a post-survey was sent via REDCap to again assess their current estimated use of USGVA over 1 month’s time, confidence in their knowledge of ultrasound, and comfort with using the technology. Existing barriers to the use of ultrasound were also evaluated.
Results
Study data was analyzed using BlueSky Statistics® software and was solely the work of the authors. The primary aim of increasing the use of ultrasound by 20% from baseline was exceeded with a pre-education combined estimated use of 81 times and a post-education estimated use of 133 times. This is a 64% increase in use (see Figure 1).
Pre- and post-survey results were analyzed using the Wilcoxon paired-sample test. A p-value of < 0.05 was used to determine statistical significance. Results from the secondary aims revealed a statistically significant improvement in how each CRNA perceived their comfort (p = 0.0004) (see Figure 2), knowledge (p = 0.008) (see Figure 3), and confidence (p = 0.0003) (see Figure 4) using ultrasound technology.
Barriers preventing volunteers from utilizing ultrasound changed from pre- to post-intervention. Before the education, participants reported more internal barriers such as lack of skill, knowledge, and training. Following the education, less internal barriers were reported but external barriers remained, such as ultrasound availability, lack of time before a case, and current work culture (see Figure 5).
Post-education results show a large decrease in education related reasons (blue colors) such as lack of skill, lack of knowledge, and time needed to train.
Participant knowledge was also assessed within the online module with 10 questions pre- and 10 questions immediately post-completion of the module. The McNemar’s test was used to compare the pre- and post-tests and a p-value of <0.05 indicated statistical significance. All questions revealed an improvement in knowledge with 6 of the questions showing a statistically significant difference (see Table 1).
Discussion
This QI project addressed the need for ultrasound education as identified through barriers by CRNA participants. This project adds to current literature on the successful use of a structured online learning module enhanced by hands-on simulation-based training. This project led to increased use of ultrasound by CRNAs through increased knowledge, comfort, and confidence. This project also decreased individual barriers through education and training.
Much of the literature detailing educational projects like this one focused on first attempt success rates as a primary goal.2–4,16–22 This QI project did not compare first attempt success rates using traditional methods versus ultrasound guidance. As previously discussed, outcomes among novice practitioners using ultrasound may not show increased first attempt success or decreased time to cannulation due to the steep learning curve necessary to become proficient in USGVA.11 This may deter those who are already successful with traditional vascular access methods to trial USGVA considering they may initially struggle.
It was difficult finding time, space, and support during the work week to complete the hands-on training. Allowing the hands-on practice to occur within a reasonable amount of time following the education, CRNA participants used personal time on 1 of 2 days to complete the hands-on simulation-based training within the project’s pre-determined timeline.
Through pre- and post-surveys, CRNAs self-reported their use of ultrasound over 1 month’s time. The authors are aware that this data is subjective and there is potential for bias considering no true measurement was used. Having participants estimate their use was the only feasible measurement option as the electronic medical record is not routinely used to document ultrasound use and the CRNA population is too large to incorporate observation-based measurement in a project of this caliber.
In a busy, constantly changing healthcare environment, CRNA retention was challenging. Throughout the project’s many phases, CRNAs retired, changed departments, and ended employment altogether. Many other volunteers completed only a portion of the project with some completing no portions at all. Because of this, the participant group was not as robust as initially planned but still exceeded the minimum sample size as determined by the a priori analysis. Various methods were employed to keep participants active and involved including frequent in-person and email communication and providing treats during simulation-based training sessions.
Other barriers to ultrasound use were identified through the project’s pre- and post-surveys and offer opportunities for future QI work. These include items such as lack of access to an ultrasound machine, lack of time before the case, conflict with other specialties or groups when choosing to use ultrasound, and current work culture. These barriers are unique to this institution and may differ when compared to barriers at other institutions. A thorough identification of barriers should be performed if this project were to be duplicated at an outside institution. Limitations to this project include the inability to measure any level of CRNA competence in USGVA which would require a formal measuring tool and supervision by a designated evaluator during clinical performance when using USGVA.
Conclusion
Through the implementation of a structured ultrasound education program, we aimed to assess the impact on participants’ utilization with a primary objective of increasing ultrasound use by 20%. At 6 months following the formalized education, the participants’ use had increased to 64%. Pre- and post-education test results revealed significant improvements in participants’ ultrasound knowledge. Furthermore, participants reported increased comfort and confidence after receiving the training. Findings highlight the efficacy of a structured ultrasound education program in enhancing both utilization rates and participants’ knowledge and skills. These results emphasize the importance of continuous education and training in healthcare settings to improve patient care outcomes and staff satisfaction.