Background, Significance, and Description of the Problem
Of the more than 100 million patients who have surgery each year, approximately 89% complain of post-surgical pain.1 When patients experience pain after surgery, their morbidity and mortality risk increases, as do hospital costs.2 Short-term pain after surgery has traditionally been treated with opioids, which decreases pain but can also produce negative side effect such as sedation, hypopnea, nausea, constipation, and opioid addiction.2
Implementation of regional anesthesia techniques are one approach to decrease the need for post-operative opioids. Regional anesthesia is a type of pain management for surgery that numbs a portion of the body.3 When regional anesthesia is administered, ultrasound guidance can improve the visualization of the patient’s anatomy for optimal placement of medications and decrease the risk of local anesthetic systemic toxicity and nerve damage.4 Ultrasound-guided regional anesthesia (UGRA) has many benefits, including a reduction in postoperative pain and opioid use, as well as more positive patient outcomes, including decreased incidence of postoperative nausea and vomiting.4 Ultrasound-guided regional anesthesia can also aid in reducing the patient’s time to discharge.4 Patients who undergo UGRA resume normal activities and rehabilitate sooner than patients who receive opioids for pain.4 Overall, UGRA increases patient satisfaction and outcomes.4
Despite its many benefits, anesthesia providers in the region assessed may lack confidence in performing UGRA due to a deficiency of exposure and experience. Ultrasound simulation training is essential for enhancing UGRA skills during student registered nurse anesthetist (SRNA) education.5–8 A systematic review found that simulation-based UGRA training significantly outperformed alternative methods, especially when compared to didactic instruction alone.5 Notably, UGRA knowledge showed significant improvement when didactic teaching was combined with simulation. This process improvement project aimed to improve SRNA confidence through a combination of increased simulation training and didactic education in UGRA techniques. Confidence levels were measured before and after participating in ultrasound simulation sessions designed to improve UGRA performance. The goal was to enhance SRNA education at a large public research university, preparing SRNAs with the essential abilities necessary for clinical excellence.
Needs Assessment
South Carolina’s largest private, non-profit healthcare system was the primary educational site for this nurse anesthesia program. Approximately 30 SRNAs graduate from this program annually, and they are required by the Council on Accreditation of Nurse Anesthesia Educational Programs to have experience in regional anesthesia.9 However, the healthcare institution currently does not allow Certified Registered Nurse Anesthetists (CRNA) to perform regional anesthesia and the SRNAs must receive their regional anesthesia training from providers outside this organization who perform UGRA. This obstacle limits SRNA exposure to UGRA cases making it difficult to build confidence in performing UGRA. Accordingly, ultrasound simulation education is needed to optimize the educational experience for SRNAs who have limited clinical experience in regional anesthesia.
To further assess the need, CRNAs in the affiliate clinical site educational system were surveyed on their confidence and education in UGRA. The survey used a Likert scale and was distributed to CRNA groups where the majority of SRNAs received their UGRA training. Of the respondents (n = 10), 80% of CRNAs reported that they felt unprepared to perform UGRA when they graduated from their nurse anesthesia program. Notably, 100% (10/10) of the respondents agreed that it would be beneficial to provide an ultrasound simulation for SRNAs prior to their entering clinical residency. Of those CRNA respondents, 50% (5/10) have been practicing for less than 10 years, and during their educational process, 80% (8/10) received less than 5 hours of ultrasound simulation education. Most notably from the survey, none of the CRNA respondents felt adequately prepared to perform UGRA when they graduated.
Scope of the Project
This project investigated whether simulated ultrasound education, compared to didactic education alone, is associated with an increase in SRNA confidence to perform ultrasound visualization of nerve anatomy at this institution. The simulation training educated SRNAs on how to recognize and interpret ultrasound imagery that identified specific nerve bundles and to relate those anatomical sites with locations where peripheral nerve blocks were placed for UGRA. The project surveyed SRNAs’ self-perceptions of their ultrasound skill level before and after participating in the simulation education.
The SRNAs received 2 didactic education lectures that fully encompassed all aspects of UGRA and peripheral nerve block techniques. Implementation consisted of three phases. In Phase 1, the project leader administered a survey to SRNAs that addressed their perceived ability to properly visualize nerve anatomy via ultrasound images provided in a textbook. In Phase 2, the SRNAs attended a 4-hour simulation session on UGRA techniques, focusing especially on visualization and interpretation of key nerve anatomy via ultrasound. In Phase 3, the project leader surveyed the SRNAs following the simulation to assess their perceived confidence for visualizing nerve anatomy with ultrasound and relating that new knowledge to UGRA. Data from the pre- and post-intervention surveys were compared to determine if perceived confidence improved after one 4-hour UGRA simulation session.
Potential Threats and Barriers
Potential challenges in implementing this project included limited access to simulation facilities and ultrasound machines, which could restrict the ability to effectively train an adequate number of SRNAs. These barriers were overcome by proper preparation and scheduling of appropriate equipment and location. A threat to this project was the possible lack of participation from SRNAs. To overcome this threat, the simulation session was well advertised and encouraged. A resistant workplace culture was the biggest challenge anticipated for implementation of this project, and thus a coalition was developed to create and implement a detailed strategic plan for the project. In accordance with the mission of the university to provide compassionate patient care, the focus was placed on education within the team.6
Synthesis of the Literature
A search was conducted for relevant literature about the education process, benefits of simulation education, and ultrasound education. Several studies5–8 described the structures needed for an effective education process, and several5–8 addressed the positive outcomes of simulation education. Many studies focused on the benefits of ultrasound education, including Hocking et al7 who argued that an ethical skills-based education in ultrasound-guided needle placement should be gained in a simulation environment before performance of nerve blocks on patients in clinical practice.
Education Process & Assessment
Across the literature, different educational methods were used to teach simulated programs, including face-to-face simulation-based education and blended-learning curriculum that incorporated the addition of online simulation components.5,8 Laurent et al6 created a checklist and assessed validity and interrater reliability of simulation training, and Kiener et al10 distributed the Comfortability in Learning Scale and Instructional Affect Assessment Instrument to examine the role comfortability played in the process of advanced learning.
Simulation Education
Chen et al5 compared simulation education and didactic education, concluding that simulation-enhanced learning is effective for acquiring new knowledge and skills; the researchers suggested that a shortened learning curve occurs when acquiring a new skill by learning with simulation. Many studies5,6,8,11 found that simulation education correlated with an increase in skills and competence among both SRNAs and practitioners.
Of the studies that compared simulation teaching methods, 4 studies5,6,8,11 revealed that simulation, compared to didactic education, was a better method of teaching technical skills that require a hands-on approach; however, the studies focused on different outcomes. In a study of 20 clinicians, Laurent et al6 found the introduction of testing into simulation-based skill training courses had a positive increase in the learning outcomes. Kiener et al11 found that SRNAs who are self-regulated can assess their strengths and weaknesses and implement strategies to improve learning; learning characteristics such as persistence, curiosity, enthusiasm, and enjoyment of learning were attributed to SRNAs’ learning success. Similarly, Lee Wiggins et al8 reported that simulation education among CRNAs was effective in teaching essential clinical skills, preparing them for future practice.
Ultrasound Education
Three studies5,7,11 evaluated ultrasound education with simulation. In a systematic review, Chen et al5 found that simulation-enhanced UGRA training was significantly more effective than alternative teaching methods compared with didactic teaching and that UGRA knowledge and skills significantly improved with simulation training. Kiener et al11 found competence in UGRA by assessing the internal perception of the clinician’s experience and comfortability. Only 1 study focused on needle placement proficiency; Hocking et al7 reviewed the benefits and pitfalls of using phantoms, anechoic, gelatin, blue phantoms, and fresh-frozen cadavers, to teach ultrasound-guided needle placement and decipher which provided a more realistic learning experience. The researchers reported that phantoms allowed repeated practice of ultrasound-guided needle placement without risk to patients, leading to improvements in both operator accuracy and efficiency along with increased confidence among practitioners.7
Implementation
Guided by the ACE Star Model of Knowledge Transformation,12 the project had 2 components of implementation: (1) the development of a self-assessment survey and (2) intervention/simulation implementation. The project was granted an Institutional Review Board (IRB) exemption by the SRNAs’ university, indicating that IRB approval was not required.
Component I: Development of Self-Assessment Survey
To assess the outcomes of the intervention, the project leader needed a measuring tool to assess confidence of the project. A thorough search was conducted to identify a validated self-assessment survey suitable for this project. Unfortunately, no existing survey met the specific parameters required. As a result, the design of Unver et al’s13 survey served as a reference framework for the creation of a new tool tailored to assess confidence specifically for this initiative.
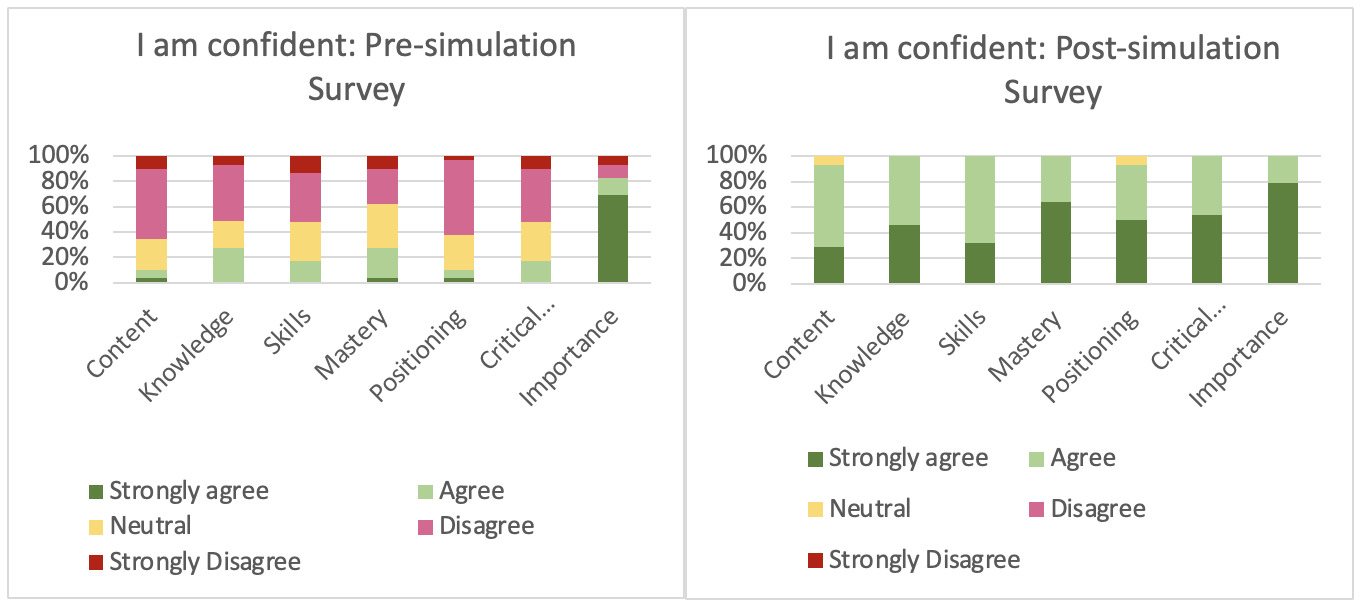
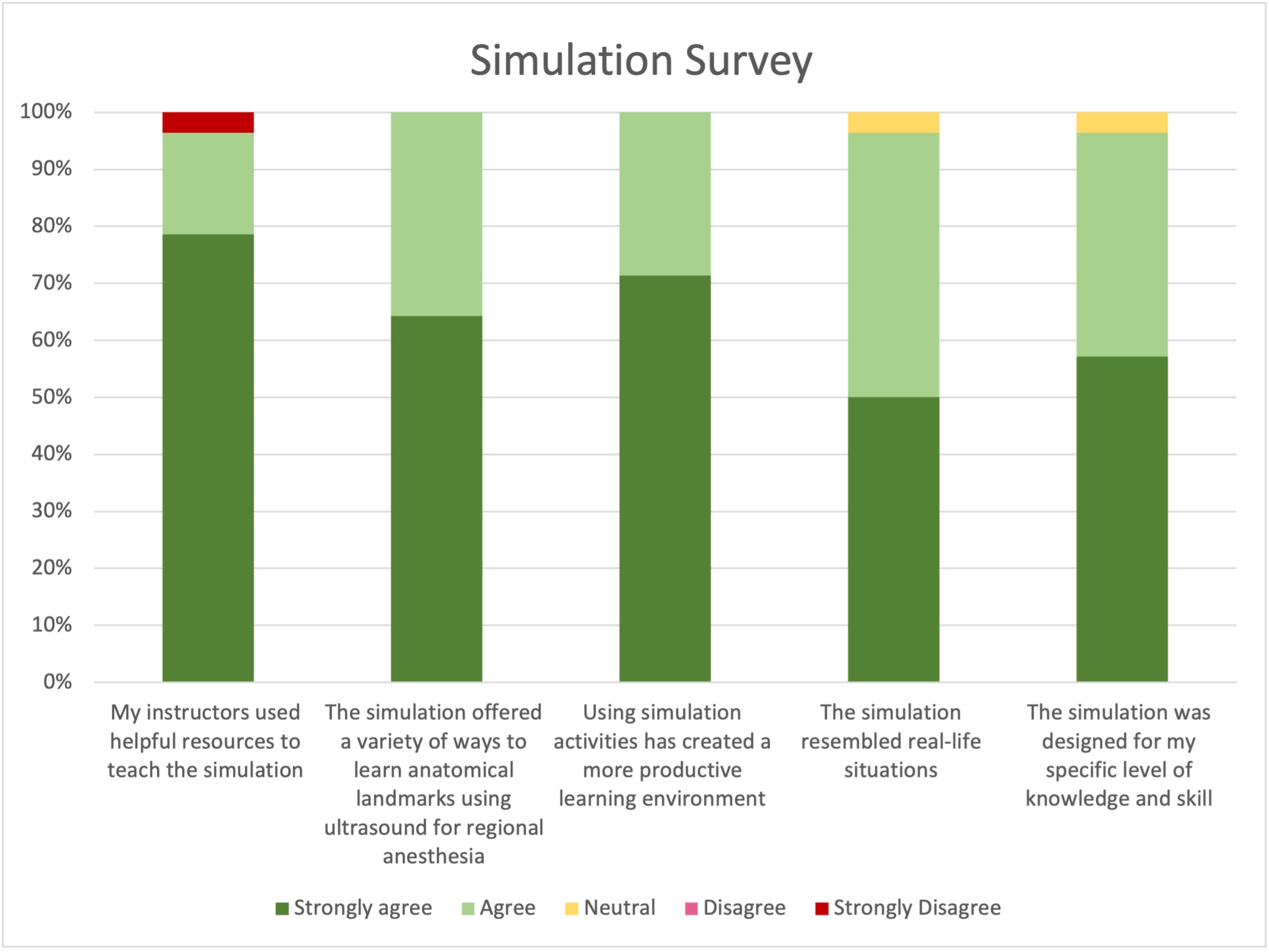
The project leader created a pre- and post-survey model to: (1) evaluate the effectiveness of the didactic education, (2) establish the baseline level of confidence, and (3) compare confidence levels before and after simulation. The pre-simulation survey included 7 questions assessing confidence with ultrasound imagery following didactic education. The post-simulation survey repeated these 7 questions and added 5 more questions related to the simulation-based education (see Table 1).
The SRNAs were provided a QR code prior to each simulation session, and the SRNAs were asked to complete the survey using their cellular phones or tablets. Ten minutes were allotted for the survey to be completed. After each simulation session, a QR code was provided on the projector screen for the post-simulation survey. The SRNAs were encouraged to complete the survey prior to leaving, but it was not a requirement.
Component II: 4-Hour Ultrasound Simulation Session
The simulation sessions took place at 2 different simulation centers, on 2 separate days. A total of 28 SRNAs were in attendance. In the first session, 17 SRNAs (divided into groups of 3-4 participants) rotated through 4 ultrasound stations, with a standardized patient at each non-invasive station. The 4 standardized patients were hired to participate, and the criteria for each patient included different body mass indexes with a focus on body habitus, to provide ultrasound education with different types of anatomy. There were 5 stations, and the fifth station was a station set up with ultrasound, a peripheral nerve needle, and a gel mold to practice needle manipulation with ultrasound. The second session, held 3 days later, was conducted with 11 SRNAs in attendance and 2 standardized patients. The process for the simulation mirrored that of the first session, with the same objectives, modules, and schedule.
The simulations were organized into 3 modules, that included all 5 stations, to focus on upper body, lower body, and trunk scanning. The upper body module focused on the brachial plexus, with the greatest emphasis on interscalene and supraclavicular nerve anatomy. The lower body module focused on the sciatic and saphenous nerve anatomy with the emphasis on the saphenous nerve at the adductor canal and the bifurcation of the tibial and common peroneal nerves at the popliteal fossa. The third module focused on trunk block locations with emphasis on erector spinae plane block and transverse abdominus plane block. During the third module, since nerve anatomy is not visualized with plane blocks, emphasis was focused on locating the preferred spot to visualize spread of local anesthetic.
Data Analysis and Results
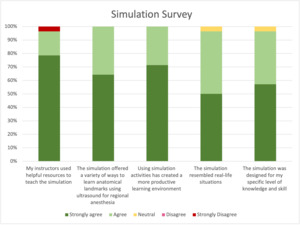
A total of 28 SRNAs attended the simulation sessions, and all completed the pre- and post-simulation surveys. The results of the surveys indicated that simulation for UGRA education builds confidence in SRNAs. In comparing the pre- and post-simulation survey results, reported confidence increased in all domains, as recorded in Table 1. In response to Q1, mastering the content of UGRA, SRNAs’ agreement increased from 10.3% to 92.9%. On the pre-survey, 27.6% agreed with Q2 and 20.7% felt neutral; post-simulation, 100% agreed with the development of knowledge to perform UGRA. When the SRNAs were asked about mastery for UGRA (Q3 & Q4), 100% agreed in both domains post-simulation. The importance of regional anesthesia and the ability to perform UGRA has been explained, and when the SRNAs were asked if “having strong ultrasound skills to be efficient in UGRA is important to me,” pre-simulation, only 24 SRNAs agreed, however, post-simulation all 28 SRNAs agreed (see Figure 1a, Figure 1b). This question highlights the significance of early exposure to UGRA for SRNAs. Recognizing the importance of this proficiency and the benefits of hands-on experience early in training is crucial for SRNA development.
The post-simulation survey included questions about the experience of the ultrasound simulation education sessions (See Figure 2). From the questions, the SRNAs agreed 100% that the simulation offered a variety of ways to learn anatomical landmarks using ultrasound for regional anesthesia, and they agreed 100% that using simulation activity created a more productive learning environment. We also learned that 96.4% agreed that simulation resembled real-life situations. With this strong response for simulation education, we have support for the addition of simulation to UGRA education curriculum.
Discussion
Based on data, simulation education for UGRA does appear to increase confidence in SRNAs. To make the data applicable to other institutional contexts and effective to future practice, this section will identify the strengths and limitations for project implementation, areas for further research, significance to nurse anesthesia, and dissemination to the field of nurse anesthesia.
Strengths and Limitations of Project Implementation
The most notable strengths of this project involved access to advanced technology, an advanced ultrasound educator, and the project’s sustainability. The project leader was able to obtain the most up-to-date ultrasound machines for the SRNAs to perform the simulation sessions, which sets this project apart from others with out-of-date technology. Despite using less advanced ultrasound equipment, other studies have demonstrated favorable outcomes with ultrasound simulation. A notable strength of this project is its replicability and sustainability for future educational initiatives. With access to a qualified ultrasound educator, the project can be easily reproduced to enhance training programs.
The project leader and advisors identified three limitations to this project’s design. First, the survey did not account for the wide range of the SRNAs’ previous exposure to UGRA. This information would be helpful in determining whether some survey answers were skewed from this knowledge. Second, this project’s results would be more generalizable with a larger sample size. The project was implemented at a single academic institution with 28 SRNA participants; a larger population and geographical participant range would strengthen the validity and increase confident claims applying to other institutional sites. Third, the 2 sessions were not identical and were distinct sessions. They did not mirror each other because the second session had 7 fewer participants and 2 fewer body habitus stations.
Areas for Further Research
In addition to extending simulation education to other sites, future research is needed to investigate long-term outcomes of simulation education and how confidence with UGRA carries into clinical practice. In this project, SRNAs were surveyed regarding their comfort with UGRA immediately following the simulation session. Further research could evaluate these outcomes after graduation, when new CRNAs are working in their clinical profession.
Significance of the Outcomes
With the opioid epidemic and the need to decrease the use of opioids in surgical settings, UGRA is important in the future of anesthesia. Graduating SRNAs with the knowledge and confidence to perform UGRA could have a large impact on the anesthesia environment, thereby improving patient care. Secondary outcomes could also be influenced from an increase in self-efficacy and confidence, increases in practice preparedness, practice satisfaction, and a decrease in professional turnover.
Conclusion
The need for skilled UGRA practitioners will continue to grow in healthcare. To support that need, SRNAs must graduate with confidence and the proper tools to perform UGRA independently. It is well documented that simulation improves the student learning environment, most significantly with hands-on training. In this project, SRNAs’ self-efficacy outcomes successfully established an improvement in SRNA confidence with basic UGRA knowledge. The results of this project lend support for a curricular process change at this project site for the inclusion of ultrasound simulation education prior to SRNAs gaining UGRA clinical experience.